Breast cancer patient in both physical and emotional pain
I choose to give this story because it still bothers me 4 years down the road. My name is Linda and I am a critical care nurse in a big city in America. Breast cancer patient hurts both physically and emotionally, something we deal with everyday especially being a cancer center hospital.
Four years ago I took care of a young 35 years old lady with end stage metastatic breast cancer. This day still remains fresh as if it happened yesterday. For those of you who are in healthcare, I beg you to stand firm and advocate for your patients as if you are fighting for one of your own.
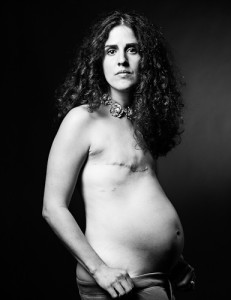
 My 35 years old had been fighting breast cancer well over five years. This time, her best ever fighting spirit was on all time high. Her breasts were scarred, full of flaps and patches. Some of the scars show they had dehisced and repaired leaving heartbreaking scars. But that was not the toughest battle yet.
My 35 years old had been fighting breast cancer well over five years. This time, her best ever fighting spirit was on all time high. Her breasts were scarred, full of flaps and patches. Some of the scars show they had dehisced and repaired leaving heartbreaking scars. But that was not the toughest battle yet.
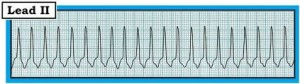
On this night, she was transferred from oncology unit to ICU after a round of Chemo. For those familiar with inpatient healthcare protocols, a patient whose oxygen saturation drops below 90%, change in mentation, heart rate in 130’s meets the criteria of being admitted to intensive care unit (ICU). On top of that her liver profile looked really bad. Her skin color was yellow due to liver failure secondary to metastasis. Excuse me if I sound too much like a text book nurse.
Series of radiological tests were performed to make sure she didn’t have a collapsed lung or pulmonary embolism. These tests showed nothing way out of normal and the oncologist together with intensivist gave me orders to continue watching the patient. The patient vision had been taken away by chemo and the only good special sense she had was hearing. She could easily recognize me because of a foreign accent.
 The heart rate kept on going up and orders to give her fluids and Morphine were executed. My eyes could not hold tears anymore and I became a bitter empathetic nurse taking care of a near helpless patient. Few hours later, I sent a specimen for complete blood count to the lab and her white cells count was near ZERO. We put the patient on neutropenic precautions, simply meaning anyone is a danger to the patient as she had no immune defense left in her system.
The heart rate kept on going up and orders to give her fluids and Morphine were executed. My eyes could not hold tears anymore and I became a bitter empathetic nurse taking care of a near helpless patient. Few hours later, I sent a specimen for complete blood count to the lab and her white cells count was near ZERO. We put the patient on neutropenic precautions, simply meaning anyone is a danger to the patient as she had no immune defense left in her system.
My patient had no family close to her, just a few friends that came to see her, one of them, a Briton. Now in neutropenic precautions, no one was allowed to stay in that room for long and a safe distance from the patient was enforced. The heart rate kept going up and up and now it’s almost 0200 AM. This time, I am dealing with heart rate of 160-180 beats per minute. The heart cannot withstand this rhythm/rate for too long before it gives up and so I had to act and act fast.
Numerous calls had been placed to the oncologist as the patient kept complaining and crying of pain. The dose I had initially was for morphine 2 mg every hour as needed. The second call I placed, the dose was doubled to 4 mg every hour as needed for pain. This did not make a difference,
The oncologist was getting irritated because of my endless calls at late hours of the night, but I was not going to give up on this lovely lady. The oncologist argument was that the patient oxygenation was poor and may potentially have lungs related problem. He was also concerned that due to liver involvement, the metabolism of opiates may be poor and this could further compromise breathing and oxygenation.
For those in healthcare, especially nurses and doctors, I am sure you can follow me on this and agree it is a true prudent rationale from the oncologist. The oncologist consulted the cardiologist and he ordered adenosine push to correct supraventricular tachycardia (heart rate above 150).
Before I could even fax the order to the pharmacy, the patient called. She could barely talk. She said “Linda, I want you to get lethal injection and kill me or get a baseball butt and hit my head so I won’t have to feel this.
 My courage, empathy and bitterness rose to the threshold that I could not hold anymore. I placed another call to the already upset oncologist, this time with demands, not requests. A frustrated voice answered the phone and I started…
My courage, empathy and bitterness rose to the threshold that I could not hold anymore. I placed another call to the already upset oncologist, this time with demands, not requests. A frustrated voice answered the phone and I started…
“I need better pain control for this patient from you right now, or else, you come in and take care of her. I need strong medications for pain and if she cannot support her airway, better be on a ventilator (life support machine) that suffer like this. I need dilaudid (hydromorphone) drip in Patient Controlled Analgesia (PCA)”.
The oncologist had never heard someone come that strong to a point of demanding which drug they want. He replied…calm down. Go ahead and start dilaudid PCA …..” Give the patient 2 mg push now before starting the drip….”. In 2 minutes, I pushed the 2 mg and the heart rate dropped quickly from 180, 150, 110, 80 and before it got to 60, the whole team was at the door with crash cart. We all thought the patient heart had given up.
At heart rate of 70, the patient stabilized. Blood pressure improved. Breathing rate lowered from 40’s to low 20’s. Her oxygen saturation went up to above 95%. We changed her from 100% non-rebreather mast to 2 liter nasal canula. She was in pain and now her pain is under control.
15 minutes later, she asked for ice water. She drank. She then requested extra blankets and off she slept. She was in pain but no one thought of pain as the reason why all her vital signs were off the limits. No adenosine for her.
Good night sunshine. You are my hero. 3 days later when her white count was starting to come back up, she passed on. She came to an end of her pain. I attended her burial and to this day, I still feel it like my own family.
Again, Good night sunshine and rest in peace.


 “Breast cancer is not a Pink Ribbon”. Please say that out loud and tell it to your friends…
“Breast cancer is not a Pink Ribbon”. Please say that out loud and tell it to your friends… Breast is the greatest symbol of femininity in all mammals. In many mammals, the only way to tell the physical difference between a male and a female is the mammary glands AKA breast, or udder in four-legged animals. Breast cancer specifically affects the greatest symbol of femininity tearing down and shattering many women definition of beauty. Cancer treatment, even worse takes away the most prominent feminine features of human beings like hair, eye lashes, breast, skin and nails.
Breast is the greatest symbol of femininity in all mammals. In many mammals, the only way to tell the physical difference between a male and a female is the mammary glands AKA breast, or udder in four-legged animals. Breast cancer specifically affects the greatest symbol of femininity tearing down and shattering many women definition of beauty. Cancer treatment, even worse takes away the most prominent feminine features of human beings like hair, eye lashes, breast, skin and nails.
 Breasts are normally obscured in non-pornographic photography/media but David defied the norms and used his photography to show how women look after mastectomy. Rather than demoralizing, David’s photography is empowering and creating a
Breasts are normally obscured in non-pornographic photography/media but David defied the norms and used his photography to show how women look after mastectomy. Rather than demoralizing, David’s photography is empowering and creating a To me, these SCAR project pictures show a new shift in society’s acceptance of a tribe of scarred, breastless and one breasted women. It is a high time we start accepting SCARRED women are just as beautiful since 1 in 8 women will be diagnosed with breast cancer at some point in their lives. This new tribe inspired by David is growing and will at some point in future became the norm, just the same way we no longer see pregnant women as unattractive. This exposure will help women to accept what we might not be able to change. Perhaps fashion designers will soon start making bras for women with one breast and accept them as “normal.” What if not having breasts or having one breast became acceptable? What if mastectomies and scarred breast are seen as a symbol of honor and strength? What if the society could tone down the breast obsession with breasts just a little bit and appreciate David work on SCAR project for pioneering the new “normal” for breast cancer fighters and survivors?
To me, these SCAR project pictures show a new shift in society’s acceptance of a tribe of scarred, breastless and one breasted women. It is a high time we start accepting SCARRED women are just as beautiful since 1 in 8 women will be diagnosed with breast cancer at some point in their lives. This new tribe inspired by David is growing and will at some point in future became the norm, just the same way we no longer see pregnant women as unattractive. This exposure will help women to accept what we might not be able to change. Perhaps fashion designers will soon start making bras for women with one breast and accept them as “normal.” What if not having breasts or having one breast became acceptable? What if mastectomies and scarred breast are seen as a symbol of honor and strength? What if the society could tone down the breast obsession with breasts just a little bit and appreciate David work on SCAR project for pioneering the new “normal” for breast cancer fighters and survivors? The happiness of finally having a son was short-lived. Lucy’s fungating breast mass was growing bigger and bigger by the day. Her pain and suffering was becoming more and more intolerable. The mass became infected and need surgery though her health condition could not have allowed it. She could not have survived a surgery, if there was one available. Lucy was abandoned by her friends, family and lovers to die in the hospital. Meru Hospice was her new home. Doctors could not operate on her. Knowledge and resources were not there.
The happiness of finally having a son was short-lived. Lucy’s fungating breast mass was growing bigger and bigger by the day. Her pain and suffering was becoming more and more intolerable. The mass became infected and need surgery though her health condition could not have allowed it. She could not have survived a surgery, if there was one available. Lucy was abandoned by her friends, family and lovers to die in the hospital. Meru Hospice was her new home. Doctors could not operate on her. Knowledge and resources were not there. Baby Moses at 5 months old and was doing really well; he was looking bright and healthy. But it was becoming progressively difficult for Lucy to take care of him. No relative ever came to visit her. She is abandoned to die alone. She depends on relatives of neighboring patients to assist her wash her clothes, change and feed her baby.
Baby Moses at 5 months old and was doing really well; he was looking bright and healthy. But it was becoming progressively difficult for Lucy to take care of him. No relative ever came to visit her. She is abandoned to die alone. She depends on relatives of neighboring patients to assist her wash her clothes, change and feed her baby.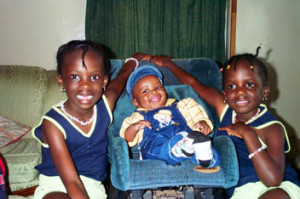










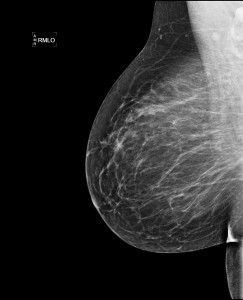 Diagnostic Mammograms are used to check for breast cancer after a lump or other sign or symptom of the disease has been found. Unfortunately, at this point, the mammogram is only used to confirm the diagnosis. This is the commonest mammogram ordered by physicians in Kenya and the rest of Africa.
Diagnostic Mammograms are used to check for breast cancer after a lump or other sign or symptom of the disease has been found. Unfortunately, at this point, the mammogram is only used to confirm the diagnosis. This is the commonest mammogram ordered by physicians in Kenya and the rest of Africa.

