What Is Patient Teaching about Breast Cancer Screening – Mammography?
- Patient teaching about breast cancer screening mammography (SM) can defined in simple terms as the process of providing helpful information to patients before, during, and after mammography. This is to increase their knowledge of the procedure and enhance their ability to cope with the procedure and related results.
-
What Patients need to know about screening mammograms:
 Patient teaching about Screening Mammogram involve: –
Patient teaching about Screening Mammogram involve: –- Teaching patients about the purpose of breast cancer screening
- The risks involved and benefits of screening mammograms
- How to prepare for mammography
- What to expect during the procedure
- Strategies for coping with the screening mammogram procedure and findings.
- Screening mammogram is the single most effective method for early breast cancer detection because it can identify breast cancer several years before physical signs and symptoms are apparent.
- Lack of screening mammograms and infrequent screening mammogram are widely recognized as major factors contributing to increased breast cancer mortality
-
How to teach patients about screening mammograms:
First time experience can be uncomfortable to many women but with correct teaching, compliance can be achieved. Teaching and motivational activities like face-to-face instruction, written materials, video presentations and pre-visit tours can be utilized to teach and support patients in learning about mammography and breast cancer screening
- Make teaching and learning an ongoing process by using combination strategies like sending a reminder letter, providing a pamphlet about screening mammograms & discussing concerns about discomfort during mammography. This has been shown to be more beneficial than face-to-face instruction only
- Use of informed decision-making process is important when promoting health screening such as screening mammogram. In educated population, research has shown that use of leaflets with decision aids appear to increase knowledge and participation in breast screening and have a positive impact on reducing decisional conflict.
-
Where does teaching about screening mammograms occur?
Patient teaching about breast cancer screening mammograms typically begins in primary care, but can also be introduced at any time of clinic or hospital visit. Public education has shown to yield the best results about screening mammograms.
- Every possible effort should be made to promote seamless delivery of patient teaching throughout the course of care and after screening mammogram.
- Conflicting information about breast cancer screening mammograms should be avoided to reduce frustration and confusion and increase
-
Who is the best to teach about breast cancer screening mammograms:
Patient teaching about breast cancer screening mammogram can be given by healthcare professionals like physicians and nurses and should not be delegated to assistive clinical staff or none clinical staff.
- Research has shown that the most effective educators of women undergoing mammography are those who individualize information to specifically address their learning needs – women just like them
-

 My 35 years old had been fighting breast cancer well over five years. This time, her best ever fighting spirit was on all time high. Her breasts were scarred, full of flaps and patches. Some of the scars show they had dehisced and repaired leaving heartbreaking scars. But that was not the toughest battle yet.
My 35 years old had been fighting breast cancer well over five years. This time, her best ever fighting spirit was on all time high. Her breasts were scarred, full of flaps and patches. Some of the scars show they had dehisced and repaired leaving heartbreaking scars. But that was not the toughest battle yet.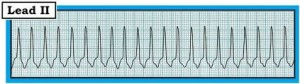 The heart rate kept on going up and orders to give her fluids and Morphine were executed. My eyes could not hold tears anymore and I became a bitter empathetic nurse taking care of a near helpless patient. Few hours later, I sent a specimen for complete blood count to the lab and her white cells count was near ZERO. We put the patient on neutropenic precautions, simply meaning anyone is a danger to the patient as she had no immune defense left in her system.
The heart rate kept on going up and orders to give her fluids and Morphine were executed. My eyes could not hold tears anymore and I became a bitter empathetic nurse taking care of a near helpless patient. Few hours later, I sent a specimen for complete blood count to the lab and her white cells count was near ZERO. We put the patient on neutropenic precautions, simply meaning anyone is a danger to the patient as she had no immune defense left in her system. My courage, empathy and bitterness rose to the threshold that I could not hold anymore. I placed another call to the already upset oncologist, this time with demands, not requests. A frustrated voice answered the phone and I started…
My courage, empathy and bitterness rose to the threshold that I could not hold anymore. I placed another call to the already upset oncologist, this time with demands, not requests. A frustrated voice answered the phone and I started…



